You have the same duty of care to your staff during this COVID-19 pandemic as you do at any other time. It will, of course, be more challenging to meet that duty. Of particular concern will be protecting their wellbeing. So how can you do that?
Prevent
In these very challenging times, being able to support your team is crucial. The World Health Organization has published Mental health and psychosocial considerations during the COVID-19 outbreak. This provides advice to a range of audiences, including team leaders and managers to protect staff from chronic stress and poor mental health during this response. Tips include:
- Ensure that good quality communication and accurate information updates are provided to all staff
- Rotate workers from higher-stress to lower-stress areas and functions
- Partner inexperienced workers with their more experienced colleagues – the buddy system helps to provide support, monitor stress and reinforce safety procedures
- Initiate, encourage and monitor work breaks
- Implement flexible schedules for workers who are directly impacted or have a family member affected by a stressful event
- Ensure that you build in time for colleagues to provide social support to each other
- Ensure that staff are aware of where and how they can access mental health and psychological support services and facilitate access to such services
- Be a good role model for self-care strategies.
See the full WHO guidance here.
Also, you could encourage colleagues to use the going home checklist at the end of their shift. The NHS poster below has been developed to encourage reflection and mindfulness at the end of each working day.

Recognise
Being able to recognise potential signs of poor mental health will help you identify those members of staff who may be experiencing difficulties.
Poor mental health can affect the way we think, feel or behave and our experiences of poor mental health, symptoms and copying mechanisms will be different.
Stress is defined by the Health and Safety Executive as ‘the adverse reaction people have to excessive pressure or other types of demand placed upon them’.
Anxiety is what we feel when we are worried, tense or afraid, particularly about things that are about to happen, or which we think could happen in the future. Occasional anxiety is normal, but if feelings of anxiety are very strong, or last for a long time, they can be overwhelming.
Potential triggers that exist in the workplace include: long working hours; not taking breaks; unrealistic expectations; high-pressure environments; unmanageable workloads or lack of control over work; poor communication; negative relationships; high-risk roles.
A change in typical behaviour can be an indicator. Symptoms will vary but there are some potential physical, psychological or behaviour indicators to look out for:
|
Physical |
Fatigue; indigestion or upset stomach; headaches; appetite and weight changes; joint and back pain; changes in sleep patterns; visible tension or trembling; nervous trembling speech; chest or throat pain; sweating; constantly feeling cold. |
|
Psychological |
Anxiety or distress; tearfulness; feeling low; mood changes; indecision; loss of motivation; loss of humour; increased sensitivity; distraction or confusion; difficult relaxing; lapses in memory; illogical or irrational thought processes; difficulty taking information in; responding to experiences, sensations or people not observable by other; increased suicidal thoughts. |
|
Behavioural |
Increased smoking and drinking; using recreational drugs; withdrawal; resigned attitude; irritability, anger or aggression; over-excitement or euphoria; restlessness; lateness, leaving early or extended lunches; working far longer hours; intense or obsessive activity; repetitive speech or activity; impaired or inconsistent performance; uncharacteristic errors; increased sickness absence; uncharacteristic problems with colleagues; apparent over-reaction to problems; risk-taking; disruptive or anti-social behaviour. |
Source: People managers’ guide to mental health at work, Mind and CIPD
Recognising when a colleague’s wellbeing or mental health may be at risk at an early stage means you can take steps to help them manage this, before it escalates.
Respond
Where you can, work in partnership with other services, including human resources, occupational health, health and safety and other services that support staff health. Know what support services exist in your organisation so that you can quickly engage them and signpost staff to them for support.
Encourage people to speak openly about how they feel. NHS Employers provides a range of health and wellbeing resources for employers. This includes an easy to use emotional wellbeing tool to help bridge a gap in understanding and enable you to talk openly and regularly about emotional health.
Mental health guidance for managers, jointly developed by Mind and the CIPD, explains, when having conversations about mental health, questions should be simple, open and non-judgemental to give the employee ample opportunity to explain the situation in their own words.
Questions to ask include:
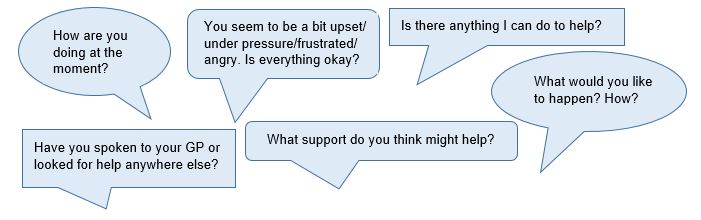
Understanding how to support staff and how to have open conversations about how they are feeling and copying will help create a positive culture around mental wellbeing. Creating opportunities for staff to feel safe talking about their mental health and how they are feeling at this time is particularly important.
Further information to help you support your staff can be found here:
World Health Organisation (WHO) – Mental health and psychosocial considerations during the COVID-19 outbreak
MIND – Taking care of your staff resources
Health and Safety Executive’s talking toolkits for preventing work related stress
Free access to wellbeing apps for all NHS staff
NHS Education for Scotland: e-learning – psychological support and wellbeing

